The human body is a complex machine with countless processes happening simultaneously to keep us functioning optimally. Among these processes is the production and elimination of various waste products. One such waste product that plays a crucial role in assessing our kidney health is creatinine.
For many of us, creatinine is just another term that appears on blood test results, often overlooked unless highlighted by our healthcare provider. But understanding what creatinine is, how it affects our body, and what its levels indicate about our health can be incredibly valuable for taking control of our wellbeing.
I first became interested in creatinine when a family member was diagnosed with early-stage kidney disease. The doctors kept referring to creatinine levels, GFR calculations, and kidney function markers. It became clear that this seemingly insignificant waste product was actually a window into the health of one of our most vital organs.
But here’s where things get confusing for many people: creatinine is often mixed up with creatine, a supplement popular among athletes and fitness enthusiasts. While they’re related, they serve very different purposes in our body. Creatine is a compound that helps supply energy to our muscles, while creatinine is the waste product that forms when creatine breaks down.
In this blog post, I’ll explore the world of creatinine – what it is, how it’s measured, what benefits it provides as a diagnostic tool, and what dangers elevated levels might indicate. I’ll also delve into the latest research from 2024-2025 that’s changing how we understand and use creatinine measurements in healthcare.
Table of Contents
Whether you’re dealing with kidney issues, have risk factors for kidney disease, or simply want to understand your lab results better, this exploration of creatinine will provide valuable insights into this important marker of kidney function. Because when it comes to our health, knowledge truly is power – and understanding creatinine is a powerful step toward better kidney health awareness.
What is Creatinine?
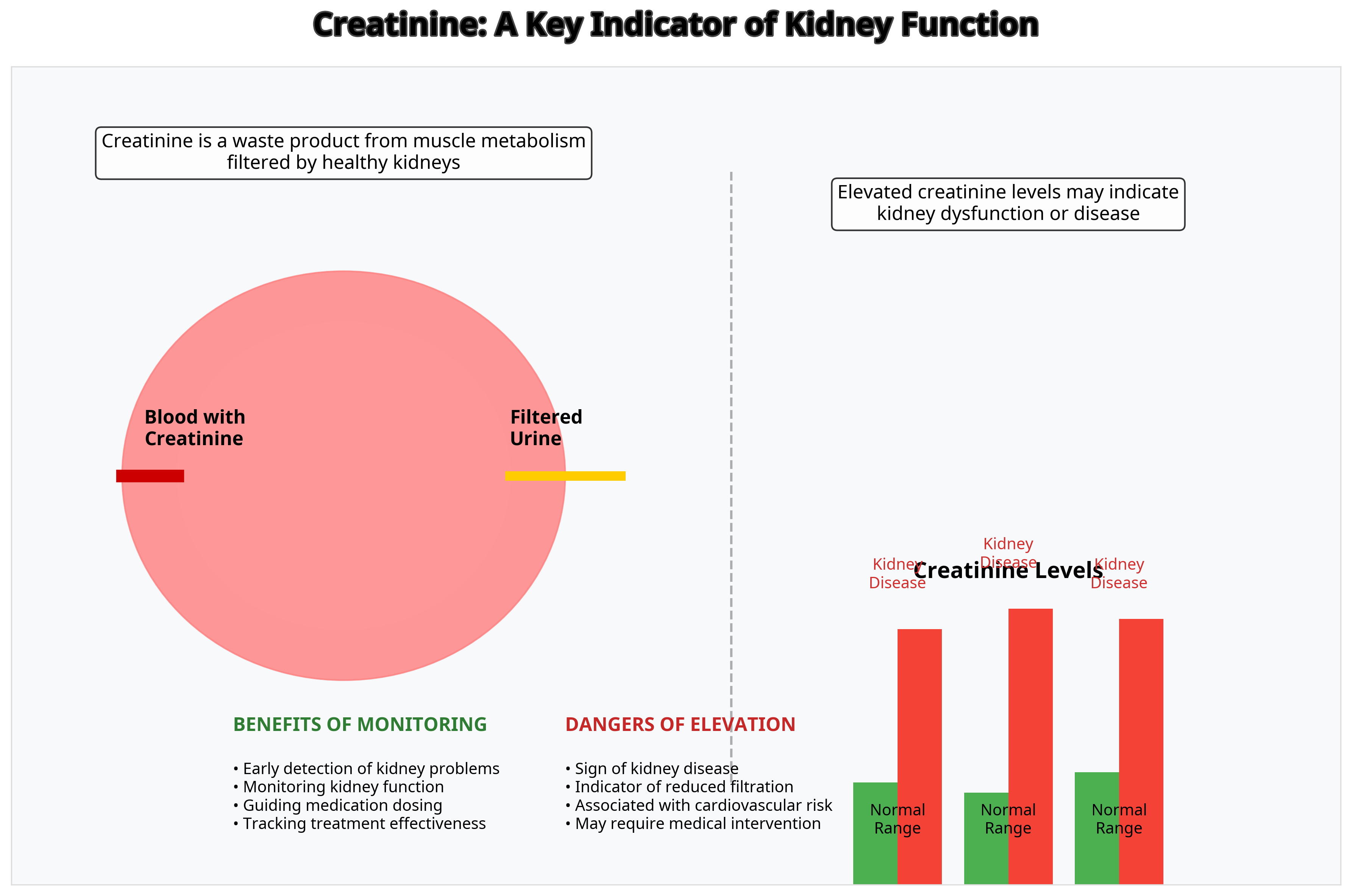
Creatinine is a waste product that comes from the normal breakdown of muscle tissue in our bodies. Every day, our muscles use a compound called creatine phosphate to provide energy for movement and other functions. As this process occurs, creatine is converted into creatinine.
The key thing about creatinine is that it’s produced at a fairly constant rate, depending on your muscle mass. This means that a person with more muscle naturally produces more creatinine than someone with less muscle. This is why men typically have higher creatinine levels than women, and why athletes might have higher levels than non-athletes.
Once creatinine is produced, it enters your bloodstream. In a healthy body, your kidneys filter this creatinine from your blood and remove it through urine. This is where creatinine becomes particularly valuable from a diagnostic perspective – it provides a window into how well your kidneys are functioning.
Creatinine as a Kidney Function Marker
The relationship between creatinine and kidney function is straightforward yet profound. Since creatinine is primarily removed from the body by the kidneys, measuring its levels in blood and urine can tell us a lot about kidney health.
When your kidneys are working properly, they efficiently filter creatinine from your blood. But if kidney function declines, creatinine begins to accumulate in your bloodstream. This is why blood creatinine levels are one of the most common tests used to assess kidney function.
However, it’s important to understand that creatinine is what healthcare professionals call a “late marker” of kidney injury. According to research from the National Center for Biotechnology Information, about 50% of kidney function must be lost before a rise in serum creatinine can be detected. This means that by the time creatinine levels are elevated, significant kidney damage may have already occurred.
To provide a more accurate assessment of kidney function, healthcare providers often use creatinine measurements to calculate the estimated glomerular filtration rate (eGFR). This calculation takes into account not just your creatinine level, but also factors like age, sex, and sometimes race or body size. The resulting eGFR gives a more precise picture of how well your kidneys are filtering waste.
Normal creatinine levels in blood typically range from 0.6 to 1.2 milligrams per deciliter (mg/dL) for men and 0.5 to 1.1 mg/dL for women. However, what’s considered “normal” can vary based on the laboratory and the specific testing method used.
Benefits of Monitoring Creatinine Levels
The primary benefit of monitoring creatinine levels is early detection of kidney problems. Regular testing can help identify kidney disease before symptoms appear, allowing for earlier intervention and potentially slowing the progression of kidney damage.
For people with known risk factors for kidney disease – such as diabetes, high blood pressure, heart disease, or a family history of kidney problems – regular creatinine testing is especially important. According to the National Kidney Foundation, early detection and treatment can prevent or delay kidney failure in many cases.
Creatinine monitoring also plays a crucial role in:
- Medication management: Many medications are processed by the kidneys and may need dosage adjustments based on kidney function. Monitoring creatinine helps healthcare providers determine appropriate medication dosages.
- Tracking disease progression: For those already diagnosed with kidney disease, regular creatinine testing helps track whether the condition is stable, improving, or worsening.
- Guiding treatment decisions: Changes in creatinine levels can help healthcare providers determine when to initiate treatments like dialysis or consider kidney transplantation.
- Evaluating treatment effectiveness: After implementing treatments for kidney disease, creatinine levels can help assess whether interventions are working.
In my own experience with my family member’s kidney disease journey, watching those creatinine numbers became a regular part of our lives. When the levels stabilized after lifestyle changes and medication adjustments, it provided tangible evidence that the treatment plan was working. This kind of measurable feedback can be incredibly motivating for patients managing chronic conditions.
Dangers of Elevated Creatinine Levels
When creatinine levels rise above normal ranges, it’s typically a warning sign that something is amiss with kidney function. Elevated creatinine doesn’t cause symptoms directly, but it indicates underlying problems that can have serious consequences if left unaddressed.
The dangers associated with high creatinine levels include:
- Indication of kidney disease: Elevated creatinine is often one of the first detectable signs of chronic kidney disease (CKD), a condition affecting approximately 10% of the global population according to a 2025 study published in Biomedicines. If left untreated, CKD can progress to end-stage renal disease, requiring dialysis or transplantation.
- Cardiovascular risks: There’s a strong connection between kidney dysfunction and heart health. Research shows that people with elevated creatinine have a higher risk of cardiovascular events like heart attacks and strokes.
- Metabolic complications: As kidney function declines, the body may struggle to maintain proper balance of electrolytes, acids, and other substances, leading to complications like bone disease, anemia, and metabolic acidosis.
- Medication toxicity: When kidneys aren’t functioning properly, medications that are normally cleared by the kidneys can accumulate to toxic levels in the bloodstream.
It’s worth noting that temporary elevations in creatinine can occur due to factors unrelated to kidney disease, such as dehydration, certain medications, or consuming large amounts of meat before testing. This is why healthcare providers typically look for persistent elevations and consider other factors before diagnosing kidney disease.
Factors That Affect Creatinine Levels
Understanding what can influence your creatinine levels is important for interpreting test results accurately. Several factors can affect creatinine levels without necessarily indicating kidney problems:
- Muscle mass: As mentioned earlier, people with more muscle mass naturally produce more creatinine. This is why athletes, bodybuilders, and men generally have higher baseline creatinine levels.
- Diet: Consuming large amounts of protein, particularly from meat, can temporarily increase creatinine levels. This is why healthcare providers often recommend avoiding meat for 24 hours before creatinine testing.
- Age: Creatinine levels can change with age, generally decreasing as we get older due to the natural loss of muscle mass.
- Medications: Certain drugs can affect creatinine levels either by changing kidney function or by interfering with creatinine measurement. Common examples include some antibiotics, chemotherapy drugs, and certain blood pressure medications.
- Hydration status: Dehydration can cause temporary elevations in creatinine concentration in the blood.
- Exercise: Intense physical activity can temporarily increase creatinine levels due to increased muscle breakdown.
- Pregnancy: During pregnancy, GFR increases, leading to lower creatinine levels in pregnant women.
I’ve found that being aware of these factors has helped me better understand fluctuations in my own test results over time. For instance, after a particularly intense workout regimen, my creatinine was slightly elevated during a routine checkup. My doctor wasn’t concerned once I mentioned my recent increase in exercise intensity.
Recent Research Studies on Creatinine (2024-2025)
The field of kidney function assessment is constantly evolving, with researchers working to improve the accuracy and utility of creatinine measurements. Several groundbreaking studies from 2024-2025 have advanced our understanding of how to better use creatinine as a diagnostic tool.
Bias-Corrected Serum Creatinine Measurements
A significant 2025 study published in Scientific Reports examined the issue of bias in creatinine measurements from electronic medical records. The researchers found that creatinine values recorded in medical records often showed a year-specific multiplicative bias that decreased over time (from a factor of 0.84 in 2007 to 0.97 in 2013).
By developing a method to correct for this bias, the researchers were able to create a more accurate dataset for tracking kidney function over time. This correction enabled a four-fold increase in the number of estimated GFR assessments suitable for kidney function research in the UK Biobank.
This research is particularly important because it allows for more accurate longitudinal studies of kidney function, which can help identify factors that accelerate or slow kidney disease progression. For patients, this means more precise monitoring of kidney health over time.
Standardized Definitions for Kidney Function Changes
In February 2025, the Journal of the American College of Cardiology published important guidelines for standardizing how changes in kidney function are defined in clinical trials, particularly for patients with heart failure.
The expert panel established that “worsening kidney function” requires a persistent increase in serum creatinine of ≥0.3 mg/dL AND a 25% increase from baseline for a specific duration. This standardization is crucial because it helps ensure consistency across research studies and clinical practice.
The guidelines also addressed the use of eGFR slope (change in eGFR over time) as a surrogate for kidney function change. While eGFR slope can be a valuable measure, the researchers noted that it poses special challenges in heart failure trials because some interventions may produce acute effects that are distinct from their long-term effects on kidney function.
For patients, these standardized definitions mean more consistent assessment and treatment approaches across different healthcare providers and settings.
Advances in Understanding Chronic Kidney Disease
A comprehensive review published in Biomedicines in February 2025 highlighted the importance of early detection of kidney injury to prevent or slow disease progression. The authors noted that many CKD patients are unaware of their condition due to its often asymptomatic nature and the low sensitivity of classic kidney biomarkers (including creatinine) for identifying early renal damage.
The review emphasized that a delay of just one year in CKD diagnosis has been associated with a high risk of progression to more severe CKD stages and eventually to kidney failure requiring dialysis or transplantation.
This research underscores the need for more sensitive biomarkers and testing approaches that can detect kidney damage earlier than traditional creatinine testing allows. It also highlights the importance of regular kidney function screening for those with risk factors, even in the absence of symptoms.
Practical Advice for Managing Creatinine Levels
While creatinine itself is a natural byproduct that doesn’t need to be “managed” directly, there are several strategies that can help maintain healthy kidney function and, by extension, healthy creatinine levels:
- Stay hydrated: Adequate fluid intake helps your kidneys function properly. The amount of water needed varies by individual, but a common recommendation is about 8 cups (64 ounces) daily for most adults.
- Maintain a kidney-friendly diet: This typically includes moderating protein intake, limiting sodium, and focusing on fresh fruits, vegetables, and whole grains. For those with existing kidney issues, working with a renal dietitian can provide personalized guidance.
- Control blood pressure and blood sugar: Hypertension and diabetes are the two leading causes of kidney disease. Managing these conditions effectively helps protect kidney function.
- Exercise regularly: Physical activity supports overall health, including kidney function. However, very intense exercise can temporarily affect creatinine levels, so it’s best to avoid strenuous workouts right before creatinine testing.
- Avoid nephrotoxic substances: Certain medications, supplements, and recreational drugs can damage the kidneys. Always discuss all substances you’re taking with your healthcare provider.
- Get regular check-ups: For those with risk factors for kidney disease, regular screening is essential for early detection and intervention.
- Be medication-aware: If you’re taking medications that affect kidney function, ensure you’re following prescribed dosages and getting recommended monitoring.
In my experience, these lifestyle modifications aren’t just good for kidney health – they support overall wellbeing. When my family member was diagnosed with early kidney disease, the whole family adopted a more kidney-friendly diet. We all benefited from the increased focus on hydration, whole foods, and reduced sodium.
My Experience with Creatinine Testing
My journey with understanding creatinine began, as I mentioned earlier, when a close family member was diagnosed with kidney disease. What started as a routine blood test revealed elevated creatinine levels, which led to further testing and eventually a diagnosis of stage 3 chronic kidney disease.
The diagnosis was a wake-up call for our entire family. We learned that kidney disease often progresses silently, with few or no symptoms until significant damage has occurred. The creatinine test had revealed a problem that might otherwise have gone undetected until much more serious complications arose.
What struck me most was how a single number on a lab report – that creatinine value – could provide such crucial information about the function of an entire organ system. It made me realize how interconnected our body’s processes are, and how important it is to pay attention to these biomarkers.
Through this experience, I’ve come to view regular health screenings not as a burden but as a valuable tool for maintaining wellness. Monitoring creatinine and other health markers gives us the power to detect problems early and take action before they become more serious.
I’ve also learned that mindfulness plays an important role in kidney health. Being mindful of hydration, diet, medication use, and other factors that affect kidney function has become second nature for our family. This awareness has led to healthier choices overall, benefiting not just kidney health but our general wellbeing.
In Summary
The journey through understanding creatinine has taken us from the basic science of how this waste product forms in our bodies to the cutting-edge research that’s improving how we measure and interpret it. Throughout this exploration, several key points stand out:
Creatinine itself isn’t harmful – it’s a natural byproduct of muscle metabolism that healthy kidneys efficiently remove from our blood. However, its value as a biomarker for kidney function makes it an invaluable tool in healthcare.
The benefits of monitoring creatinine are clear: early detection of kidney problems, guidance for medication dosing, tracking of disease progression, and evaluation of treatment effectiveness. These benefits make regular creatinine testing a cornerstone of preventive healthcare, especially for those with risk factors for kidney disease.
At the same time, we must acknowledge the limitations and potential dangers associated with creatinine. Elevated levels can signal serious kidney dysfunction that, if left untreated, can progress to kidney failure. Yet creatinine is a late marker, only rising after significant kidney function has already been lost. This underscores the importance of comprehensive kidney health monitoring that doesn’t rely solely on creatinine measurements.
Recent research from 2024-2025 has made significant strides in improving how we use creatinine measurements. From bias-corrected measurement techniques to standardized definitions of kidney function changes, these advances are enhancing our ability to detect, monitor, and treat kidney disease more effectively.
For me, the most profound realization from this journey has been understanding how our daily choices impact kidney health. The foods we eat, the water we drink, the medications we take, and the exercise we get all influence how well our kidneys function – and by extension, our creatinine levels.
I believe that knowledge empowers us to make better health decisions. By understanding creatinine and its significance, we can be more proactive about kidney health, potentially preventing problems before they start or catching them early when intervention is most effective.
Whether you’re dealing with kidney issues, have risk factors that put you at higher risk, or are simply interested in optimizing your health, I hope this exploration of creatinine has provided valuable insights. Remember that while creatinine is just one marker, it opens a window into the health of one of our most vital organ systems.
The next time you see creatinine listed on your lab results, you’ll know not just what that number means, but the story it tells about your kidney health and what actions you might take to write a healthier next chapter.
After all, in the complex narrative of our health, understanding even one character – like creatinine – can help us better comprehend and influence the entire story.
References
- National Center for Biotechnology Information. (2024). Renal Function Tests – StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK507821/
- MedlinePlus. (2023). Creatinine Test. https://medlineplus.gov/lab-tests/creatinine-test/
- National Kidney Foundation. (2023). Creatinine. https://www.kidney.org/kidney-topics/creatinine
- Gorski, M., et al. (2025). Bias-corrected serum creatinine from UK Biobank electronic medical records generates an important data resource for kidney function trajectories. Scientific Reports. https://www.nature.com/articles/s41598-025-85391-7
- Lala, A., et al. (2025). Standardized Definitions of Changes in Kidney Function in Trials of Heart Failure: JACC Expert Panel From the HF-ARC. Journal of the American College of Cardiology. https://www.jacc.org/doi/10.1016/j.jacc.2024.11.041
- Coimbra, S., & Santos-Silva, A. (2025). New Advances in Chronic Kidney Disease: Biology, Diagnosis and Therapy. Biomedicines, 13(2), 518. https://pmc.ncbi.nlm.nih.gov/articles/PMC11853119/
- Heart Age Calculator - August 12, 2025
- Home Workout Estimator - July 29, 2025
- Plant-Based Macro Calculator - July 29, 2025

